If you or a loved one faces surgery to remove the body or tail of the pancreas—a procedure known as a distal pancreatectomy—you may be a candidate for the modern, minimally invasive “keyhole” technique (Minimally Invasive Distal Pancreatectomy, or MIDP). This approach, which includes laparoscopic and robotic surgery, is strongly recommended for its patient benefits: less blood loss and a significantly faster recovery.
A major study by the Dutch Pancreatic Cancer Group, published in the Annals of Surgery, tracked the national shift toward MIDP. The findings are a huge success story, confirming that this complex surgery can be safely and effectively implemented on a national scale, with the keyhole approach growing to nearly two-thirds of all procedures.
Real Benefits for the Patient
The widespread use of MIDP delivered tangible advantages:
- Shorter Hospital Stay: Patients who underwent the keyhole operation were able to go home sooner.
- Less Blood Loss: The keyhole approach dramatically reduced blood loss during the procedure, reporting a median of 150 mL compared to 500 mL for open surgery.
- Superior Outcomes: In experienced hands, the keyhole approach was safer.
The Critical Role of a Specialist Surgeon
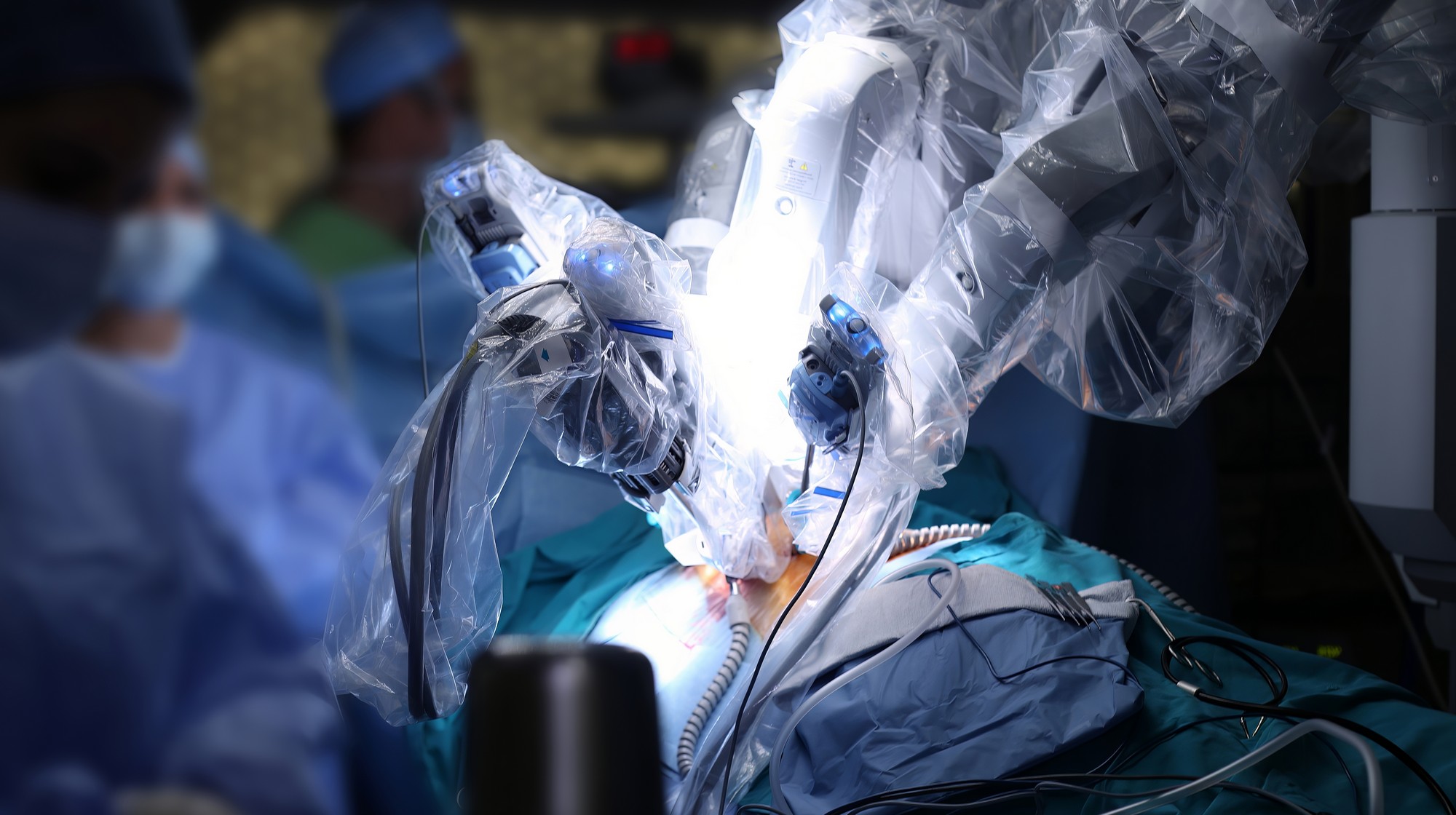
The success of a keyhole operation, especially one as intricate as a distal pancreatectomy, is deeply tied to the surgeon’s specialized training and experience. The study itself highlights this need for expertise, noting the rapid rise of robotic-assisted keyhole surgery (from 5.5% to almost 30%).
Robotic surgery, while offering surgeons incredible precision, 3D vision, and better instrument control, is a distinct technique that requires specific training. Other studies on the adoption of this technology emphasize that surgeons must complete a significant number of procedures—sometimes 85 cases or more—to move past the initial ‘learning phase’ and achieve consistently excellent results.
This is where patient choice is crucial:
- Complexity: Pancreas surgery is inherently complex due to the organ’s deep position and its close relationship with major blood vessels. While MIDP offers great benefits, it is technically challenging.
- Consistency: The Dutch study revealed a significant variation in MIDP usage among different centers (from 45% to 75% adoption). This variation suggests that not all centers or surgeons have achieved the same level of comfort and experience with the technique.
For you, the patient, this means that seeking out a surgeon who is specifically and extensively trained in minimally invasive (laparoscopic and robotic) distal pancreatectomy is highly recommended. Their experience is the greatest guarantee that you will benefit from the reduced trauma and faster recovery this modern technique can offer, while minimizing the risk of complications or conversion to open surgery.
Reference:
Korrel, Maarten MD, PhD*,†; van Hilst, Jony MD, PhD*,‡; Bosscha, Koop MD, PhD§; Busch, Olivier R.C. MD, PhD*,†; Daams, Freek MD, PhD†,∥; van Dam, Ronald MD, PhD; van Eijck, Casper H.J. MD, PhD#; Festen, Sebastiaan MD, PhD‡; Groot Koerkamp, Bas MD, PhD#; van der Harst, Erwin MD, PhD**; Lips, Daan J. MD, PhD††; Luyer, Misha D. MD, PhD‡‡; de Meijer, Vincent E. MD, PhD§§; Mieog, J. Sven D. MD, PhD; Molenaar, I. Quintus MD, PhD; Patijn, Gijs A. MD, PhD##; van Santvoort, Hjalmar C. MD, PhD; van der Schelling, George P. MD, PhD***; Stommel, Martijn W.J. MD, PhD†††; Besselink, Marc G. MD, MSc, PhD*,†; for the Dutch Pancreatic Cancer Group. Nationwide use and Outcome of Minimally Invasive Distal Pancreatectomy in IDEAL Stage IV following a Training Program and Randomized Trial. Annals of Surgery 279(2):p 323-330, February 2024. | DOI: 10.1097/SLA.0000000000005900