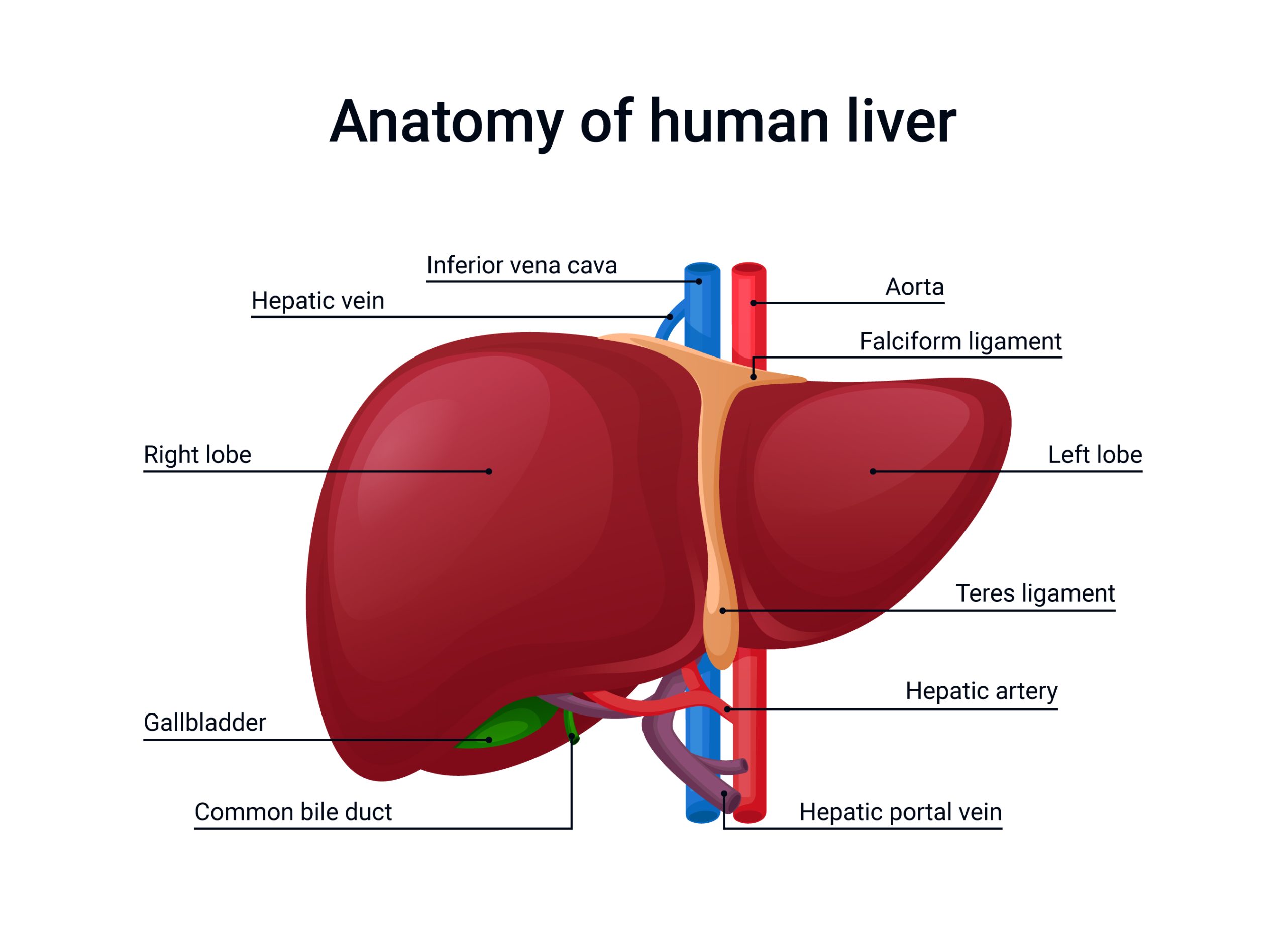
For experienced liver surgeons, the ability to visualize complex anatomy is a deeply ingrained skill. Yet, relying on traditional 2D scans for preoperative planning in complex liver resections leaves too much to chance. The human liver’s intricate vascular and segmental anatomy varies significantly from patient to patient, and a complex resection demands a detailed understanding of these individual nuances. This is where 3D reconstruction of liver imaging shines, offering a precision tool that translates into safer, more successful surgery.
The idea that expertise makes technology unnecessary overlooks a crucial point. A surgeon’s skill is best enhanced by technology. In difficult cases, such as those with tumours near major vessels or complex anatomical variations, a 3D model transforms a mental exercise into a tangible surgical rehearsal. It provides an intuitive, interactive blueprint, allowing for precise planning of resection lines and accurate calculation of the future liver remnant—a crucial factor in avoiding postoperative liver failure.
The key to minimally invasive success
This foresight is particularly valuable for minimally invasive liver surgery (MILS). The magnified but limited field of view of laparoscopy or robotic surgery can obscure the liver’s deep anatomy. The lack of tactile sensation in these procedures makes navigating the liver’s complex terrain even more difficult. A high-quality 3D reconstruction helps overcome these limitations.
- Improved navigation: By converting 2D scans into a rotatable and interactive 3D model, surgeons can precisely visualize the location of a tumour and its relationship to the surrounding vascular and biliary structures before making an incision. This is similar to having a GPS for the liver.
- Optimal approach: The 3D model helps determine the best surgical approach, especially when dealing with unusual anatomy. Some studies show that 3D analysis can alter the surgical strategy in a significant percentage of complex cases.
- Enhanced precision: When combined with technologies like intraoperative augmented reality (AR) or fluorescent imaging, the 3D model can be overlaid onto the live laparoscopic video feed. This “x-ray vision” guides the surgeon to the exact resection planes, leading to less blood loss and shorter operative times, particularly for complex cases.
Ultimately, using 3D technology is not about a lack of skill but a commitment to using every tool available to provide the safest and most effective care. It is a vital step forward in modern, personalized liver surgery.